A radiation center in Italy uses charged particles to treat cancer. The center’s synchrotron generates the protons and carbon ions needed for treatment.
Getty Images
At first, the rough patch on the roof of Mike’s mouth didn’t seem like anything to worry about. It didn’t hurt. But it didn’t go away. His dentist referred him to an ear, nose, and throat doctor, who did a biopsy, which was inconclusive.
So far, that didn’t sound so bad. But when Mike followed up with an oral surgeon, he got a diagnosis that is the stuff of nightmares: He had a rare, life-threatening cancer of the salivary gland called adenoid cystic carcinoma. Standard treatment in the United States is surgery of the palate, followed by radiation therapy.
Mike learned it would take as long as 14 hours to surgically remove the tumor, which grew rapidly to the size of a ping pong ball beneath the palate. He could lose the ability to speak or swallow, at least temporarily. Even then, he faced a high chance that the cancer would eventually metastasize, probably to his lungs. Untreated, it could spread to his brain.
“I don’t have a fear of death. It’s a fear of living badly,” says Mike, 63, an advertising professional. “That’s what drove me to find other treatment options, the fear of being a shell of myself.” (Concerned about his medical privacy, he asked to not use his full name.)
In his fear-fueled research, Mike discovered an alternative to surgery that might kill the cancer and prevent its future spread: Carbon ion therapy. Like traditional radiation, carbon ion therapy damages the DNA of fast-growing cancer cells, ultimately destroying them. But unlike older forms of radiation, this technique causes minimal harm to normal tissue. It also works against tumors that are resistant to X-ray treatment, and studies suggest it triggers an immune response against cancer.
Globally, carbon ion therapy is viewed as the next horizon of cancer care. About 22,000 patients have received the treatment at 13 centers in Germany, Austria, Italy, Japan, and China. More locations are under development in South Korea, Taiwan, and France.
Yet the therapy has followed an odd trajectory in the US. Although it was developed in California in 1975 and early research pointed to its advantages, not a single carbon ion facility, not even a research-oriented one, exists in the US. Other countries invested public money in the technology, but so far, American proponents of carbon ions have been unable to garner federal construction money or sufficient private backing.
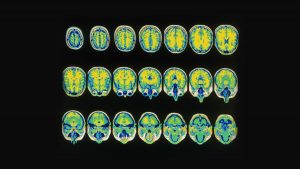
What’s flourished instead is a related approach called proton therapy, which also uses charged particles and has some of the same benefits. Today, 31 US proton centers offer treatment for cancers in areas where radiation damage to surrounding normal tissue could be dangerous or even deadly, such as tumors at the base of the skull or tumors in young children.
Carbon ion therapy is similarly precise, but because carbon ions are heavier, they deliver more cancer-killing power than protons do. Carbon centers have reported impressive survival rates, particularly for hard-to-treat bone and soft tissue cancers such as spinal tumors.
The therapy involves accelerating carbon ions to two-thirds the speed of light, then “painting” a tumor with the radiation beam. Accelerated particles deliver their energy in a sort of delayed burst called a Bragg peak, so that very little damage occurs to normal tissue as the beam enters the body in a thin stream at a high velocity, and the killing power is concentrated on the tumor, where the particle track stops. (Traditional radiation damages tissue as the beam enters and exits the body, although radiologists use techniques to minimize the damage.)
At least on the surface, the story of carbon ion therapy counters a myth about American medicine—that while Americans pay more per capita for health care than other developed countries, the US has the world’s most advanced medical technology. But are Americans in fact missing out? The nuanced answer is that no one knows for sure, because neither carbon ion nor proton therapy has “gold standard” evidence from randomized Phase III clinical trials showing patients live longer with the treatment than with standard radiation. [(Such trials are ongoing)](https://www.cancertodaymag.org/Pages/Summer2019/Focusing-on-Proton-Therapy.aspx.
“There’s a theory it’s better treatment—theory, not proven,” says Otis Brawley, an influential oncologist at Johns Hopkins University, of particle therapy. He adds that, again in theory, carbon ions ought to be superior to protons. “We should pursue carbon ion therapy,” he says. “But we should do the clinical studies to see where it is appropriate to use it.”
The trouble is in how research has been conducted so far. The highest-quality studies require patients to be randomly assigned to particle-based or standard radiation, and in most of the existing studies—in Japan, China, or Europe—researchers made that selection; it wasn’t done randomly. Different centers use different protocols, making comparisons difficult. And the lack of carbon ion centers in the US poses a logistical challenge for American researchers.
For its part, the National Cancer Institute is funding grants to uncover the properties of ionized particles. But because the particle beams produce different biological changes at different doses, untangling their effects can be challenging, says Norman Coleman, associate director of the NCI’s Radiation Research Program. In other words, it’s not just a matter of turning up the volume.
Particle-based cancer therapy evolved almost a century ago in an atmosphere of pure scientific exploration. Ernest Lawrence created the first cyclotron in 1928 at the University of California Berkeley, a circular contraption made of glass, bronze, and sealing wax that could speed the particles until they blasted apart into high-energy particles. He won the Nobel Prize for his work.
In the ensuing decades, other scientists discovered that high-energy particles could be used as a medical therapy, and that heavy ion beams could kill tumors. In 1975, Eleanor Blakely, senior staff biophysicist at the Lawrence Berkeley National Laboratory in Berkeley, California, was part of the first team of physicians and scientists to investigate the medical uses of ions.
She studied carbon, neon, silicon, and argon. Argon, for example, caused too much tissue damage. “It became a challenge of trying to figure out which one targeted the tumor with a high enough spectrum of ionization while sparing normal tissues,” she says.
Carbon and neon had similar effectiveness, she concluded. By 1988, the lab had treated 239 cancer patients with neon in Phase I and II studies. Survival rates doubled with certain advanced cancers, such as those of the salivary gland, paranasal sinus, and bone sarcoma, compared with conventional radiation therapy.
But then this line of inquiry came to an abrupt end. When the Berkeley accelerator shut down in 1993, at the end of its lifespan, there was no financial support to build another heavy ion facility. Japan took the promising Berkeley results and built the world’s first carbon ion therapy center in 1994. Blakely would like to see carbon ion treatment return to the US, even in an experimental setting. “Carbon delivers more energy, giving it a therapeutic advantage,” she says.
Twenty-five years later, Hak Choy, chair of radiation oncology at the University of Texas Southwestern Medical Center in Dallas, hopes to be the first to fill the gap in the US. He has a detailed design and plans funded by an NCI grant.
He helped structure a groundbreaking Phase III trial of carbon ion therapy for pancreatic cancer. One hundred patients from the United States, Japan, Germany, and Italy will receive free treatment in Japan. They will be randomly assigned to either conventional (photon) radiation or carbon ion therapy; one-third will receive conventional treatment and two-thirds will receive carbon. All patients also will receive chemotherapy. “This kind of (global) trial has never been done anywhere in the world,” Choy says.
Choy is optimistic he can prove the superiority of carbon ion therapy. “The assumption is that we will double the survival time, based on data from Japan,” he says.
If it’s successful, UT Southwestern will still need to find the money to build the particle accelerator. Proton therapy centers cost about $200 million; the more massive carbon ion centers run about $300 million. Carbon requires a longer pathway to reach its optimal speed in a particle accelerator and thicker shielding to prevent leakage of radiation. But Choy likes to note that a single Boeing 777 also costs about $300 million.
Despite the hurdles and the lack of data, Mike, the advertising professional, decided to pursue carbon ion therapy. He sought out a facility in Japan, one of six operating in the country, and paid $70,000 upfront for 16 treatments over four weeks.
The trek to Japan in January 2018 turned out to be a life-saver. Two weeks after returning from his treatment, he went skiing with his children and returned to work. Recently, he took a 22-mile mountain bike ride that required him to carry his bike over snowbanks. He is planning a motorcycling adventure in the Himalayas.
He doesn’t know how long he’ll be cancer-free. He also has no way of knowing how he would have ultimately fared under a different treatment. But he’s thankful to have avoided the pain and disfigurement of surgery. “All I can know is what I was faced with and where I am now, and it’s pretty damned good,” he says.
Other US patients have a long wait for the most potent radiation treatment to blast their tumors.
More Great WIRED Stories
- How the nerds are reinventing pop culture
- A “NULL” license plate landed one hacker in ticket hell
- The desperate race to neutralize a lethal superbug yeast
- Tour the factory where Bentley handcrafts its luxury rides
- How to reduce gun violence: Ask some scientists
- 👁 Facial recognition is suddenly everywhere. Should you worry? Plus, read the latest news on artificial intelligence
- ✨ Optimize your home life with our Gear team’s best picks, from robot vacuums to affordable mattresses to smart speakers.